Bariatric (weight loss) and Metabolic surgery
Bariatric surgery (or weight loss surgery or Metabolic surgery) includes a variety of procedures performed on people who are obese. Long term weight loss is largely achieved by altering gut hormone levels that are responsible for hunger and satiety. Bariatric surgery is a hormonal surgery, in which the alteration in gut hormones develops as a result of the procedure’s restriction and malabsorption.
Who is an obese person?
Obesity is defined as abnormal or excessive fat accumulation that presents a risk to health. A body mass index (BMI) over 30 is obese.
BMI = weight in Kgs/height in meter 2
WHO classification of obesity:
| Classification | BMI ( kilogram/m 2 ) |
| Underweight | <18.5 |
| Normal weight | 18.5-24.9 |
| Overweight | 25-29.9 |
| Obesity Class 1 | 30-34.9 |
| Obesity Class 2 | 35-39.9 |
| Extreme Obesity Class 3 | >40 |
What are the weight loss treatments available?
Weight loss methods for people who are obese include:
- Healthy eating
- Exercise
- Prescription drugs and natural health products
- Endoscopic procedures
- Weight loss surgery (also known as bariatric surgery)
Why bariatric surgery is called as metabolic surgery?
Because Bariatric surgery is used to treat metabolic conditions like Type 2 diabetes mellitus, hypercholesterolemia etc..
Why Bariatric/metabolic surgery is done?
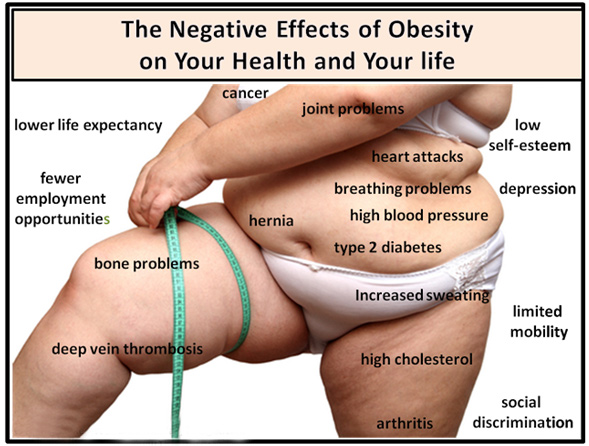
Bariatric surgery is done to help you lose excess weight and reduce your risk of potentially life-threatening weight-related health problems, including:
- Heart disease and stroke
- High blood pressure
- Nonalcoholic fatty liver disease (NAFLD) or nonalcoholic steatohepatitis (NASH)
- Sleep apnea
- Type 2 diabetes
Bariatric surgery is typically done only after you’ve tried to lose weight by improving your diet and exercise habits.
For bariatric surgery to treat diabetes:
- If you have a BMI of 35 or more with type 2 diabetes and/or other illnesses related to excess weight, and have not been able to achieve normal fasting blood sugar (less than 125 mg/dl or HbA1c less than 7 percent), you probably are a candidate for diabetes surgery.
- In some cases of inadequately controlled diabetes, patients may be eligible for bariatric surgery even if they have a BMI of less than 35.
Bariatric surgery isn’t for everyone who is severely overweight. You may need to meet certain medical guidelines to qualify for weight-loss surgery. You likely will have an extensive screening process to see if you qualify. You must also be willing to make permanent changes to lead a healthier lifestyle.
You may be required to participate in long-term follow-up plans that include monitoring your nutrition, your lifestyle and behavior, and your medical conditions.
Preparation before surgery
- Complete detailed physical examination.
- Multiple laboratory investigations to check the functioning of your organs systems like heart, kidney etc.
- You may have restrictions on eating and drinking and which medications you can take.
- You may be required to start a physical activity program and to stop any tobacco and alcohol use.
- You may also need to prepare by planning ahead for your recovery after surgery. For instance, arrange for help at home if you think you’ll need it.
How bariatric surgery is performed?
- Bariatric surgery is done in the hospital using general anesthesia. This means you’re unconscious during the procedure.
- The specifics of your surgery depend on your individual situation
- Today, most types of bariatric surgery are performed laparoscopically. A laparoscope is a small, tubular instrument with a camera attached. The laparoscope is inserted through small incisions in the abdomen. The tiny camera on the tip of the laparoscope allows the surgeon to see and operate inside your abdomen without making the traditional large incisions. Laparoscopic surgery can make your recovery faster and shorter, but it’s not suitable for everyone.
- Surgery usually takes several hours. After surgery, you awaken in a recovery room, where medical staff monitors you for any complications. Depending on your procedure, you may need to stay a few days in the hospital.
What are the types of weight-loss surgery?
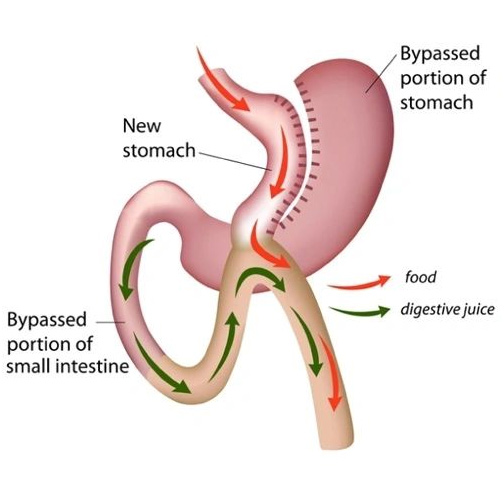
Laparoscopic Roux-en-Y Gastric Bypass
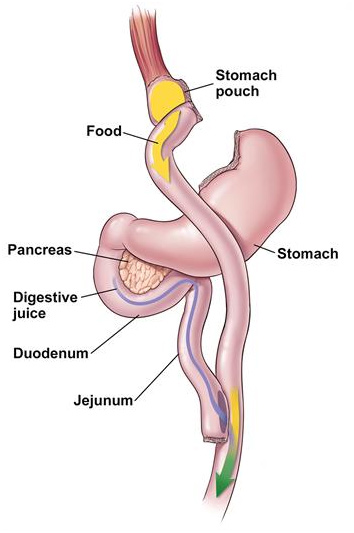
How it works: This procedure involves creating a small stomach pouch. This reduces the amount of food you can eat. The intestine is connected to the new pouch and rerouted. The pouch is connected directly to the lower part of the small intestine. Food bypasses the lower stomach, the first part of the small intestine (duodenum) and some of the second part (jejunum). The changes created during gastric bypass cause changes in the way the gut and the pancreas interact. This affects diabetes control even before weight is lost. Patients generally can return to work within three to four weeks. Gastric bypass is a good surgical option in many patients.
Laparoscopic Sleeve Gastrectomy (LSG)
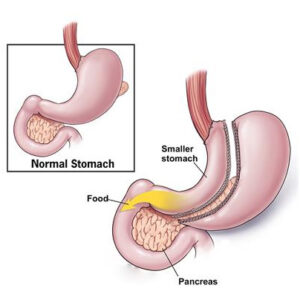
How it works: LSG reduces the size of the stomach and limits food intake. LSG is technically easier to perform than gastric bypass and is a good surgical option in many patients. Patients who are at risk for undergoing anesthesia, or who have a heart or lung problem and should not undergo a long surgery, may also benefit from this surgery. Patients generally stay in hospital for 3 to 4 days and can return to work within three to four weeks.
Duodenal Switch (DS)
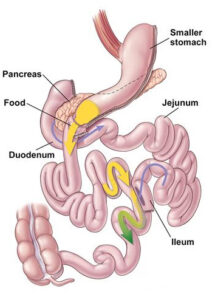
How it works: DS is another procedure that results in calories not being absorbed well. DS is a combination of LSG and a large bypass procedure. The procedure creates a smaller stomach that is connected to the farthest part of the small intestine. The duodenum, jejunum and part of the proximal ileum are bypassed and then connected to a point near the ileocecal valve. The surgery is effective, but also riskier than other procedures. It is generally only for people who have BMI higher than 50.
Minigastric Bypass (MGB)
- The new mini stomach created by the surgical procedure can only hold 4-6 ounces of food, thereby restricting the amount of food you can eat.
- The small intestine is responsible for the absorption of calories. Since a portion of the small intestine is bypassed the number of calories absorbed is drastically reduced thereby leading to weight loss.
- Also, the levels of the hormone Ghrelin which is responsible for hunger is lowered as a result of this surgery. This leads to a reduced appetite in people who have undergone this surgery
Which type of weight-loss surgery is best for you depends on your specific situation. Your surgeon will take many factors into account, including body mass index, eating habits, other health issues, previous surgeries and the risks involved with each procedure.
What are the changes in diet after bariatric surgery?
After weight-loss surgery, you generally won’t be allowed to eat for one to two days so that your stomach and digestive system can heal. Then, you’ll follow a specific diet for a few weeks. The diet begins with liquids only, then progresses to pureed, very soft foods, and eventually to regular foods. You may have many restrictions or limits on how much and what you can eat and drink.
Results of bariatric surgery
Bariatric surgeries can provide long-term weight loss. The amount of weight you lose depends on your type of surgery and your change in lifestyle habits. A majority of patients lose 50 to 80% of the excess weight during the 18-24 months after surgery.
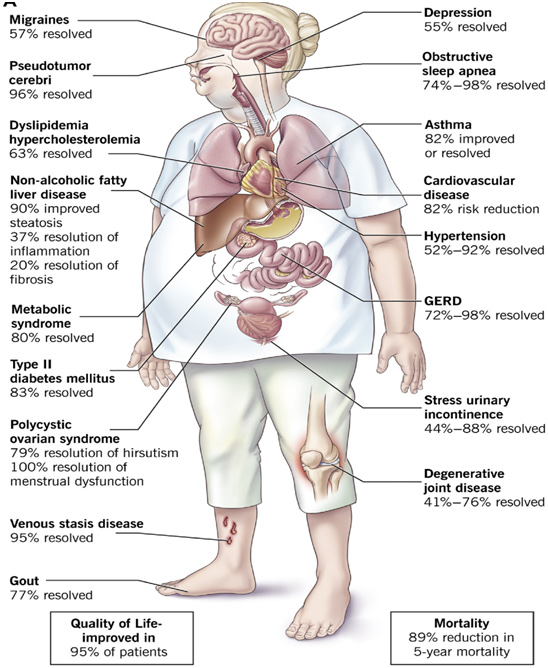
In addition to weight loss, gastric bypass surgery may improve or resolve conditions often related to being overweight, including:
- Heart disease
- High blood pressure
- Obstructive sleep apnea
- Type 2 diabetes
- Nonalcoholic fatty liver disease (NAFLD) or nonalcoholic steatohepatitis (NASH)
- Gastroesophageal reflux disease (GERD)
- Osteoarthritis (joint pain)
Gastric bypass surgery can also improve your ability to perform routine daily activities, which could help improve your quality of life.
What happens to people who underwent bariatric surgery to treat diabetes?
- Improvements to blood glucose may start right after the surgery
- You will probably be able to reduce the dosage of the diabetes medications
- You might even be able to stop taking medications entirely
- You will reduce your chances of heart attacks, strokes, and heart and kidney failures
- You might be able to stop taking medications for those conditions as well.
- Sleep apneaand fatty liver should improve.
- In particular, Roux-en-Y surgery is effective at diabetes control. About 33% of these patients do not need diabetes drugs after surgery. Within 2 years of surgery, a total of 85% of patients do not require medication. Their diabetes is in remission.
When I can return to work after Bariatric Surgery?
Depending on the type of surgery and how you heal, you can probably return to work in 3-4 weeks
When should you contact your doctor after weight-loss surgery?
In the short term, your healthcare team will provide a list of when you should contact the doctor, such as if you:
- Develop a fever.
- Have increasing pain or new pain.
- Have any issues with your incision that point to infection.
- Are constantly vomiting or unable to eat.
- Are extremely constipated.
When weight-loss surgery doesn’t work?
It’s also possible to not lose enough weight or to regain weight after any type of weight-loss surgery, even if the procedure itself works correctly. This weight gain can happen if you do not follow the recommended lifestyle changes, such as getting regular physical activity and eating healthy foods.
Risks involved in Bariatric surgery
As with any major procedure, bariatric surgery poses potential health risks, both in the short term and long term.
Short term complications associated with the surgical procedure can include:
- Excessive bleeding
- Infection
- Adverse reactions to anesthesia
- Blood clots
- Lung or breathing problems
- Leaks in your gastrointestinal system
Longer term complications of weight-loss surgery vary depending on the type of surgery. They can include:
- Bowel obstruction
- Dumping syndrome, which leads to diarrhea, flushing, lightheadedness, nausea or vomiting
- Gallstones and kidney stones formation
- Hernias
- Low blood sugar (hypoglycemia)
- Malnutrition
- Ulcers
- Vomiting
- Acid reflux
- The need for a second, or revisionsurgery or procedure (not common)
How to reduce your risk after surgery?
It is important to understand the long-term commitment required to achieve success
- Carefully follow the instructions that have been given to you after your surgery. Speak with your doctor if you have any questions.
- Permanent and significant changes to eating habits and food choices are required for bariatric surgery to be effective.
- Long-term monitoring by your doctor or dietician will be required.
What is the follow up schedule after bariatric surgery?
You will be asked to keep the scheduled appointments after the surgery
- Follow-up after surgery (generally every 1 week for one month, every 1 month for first 6months, and then once a year)
- Lab work (at 6 months, one year, and then once a year)
- Dietary counseling (at one month, 3 months and then as needed)
- Psychological counseling (at one month and then as needed) and exercise counseling (at one month and then as needed).
- Routine healthcare with your primary healthcare provider (as needed)
- Monthly support group attendance
Will insurance cover the Bariatric surgery?
As per the IRDAI’s (Insurance Regulatory and Development Authority of India) guidelines, bariatric or weight loss surgery was included under medical insurance cover. Insurers in India will have to offer weight loss surgery cover to customers purchasing policies after 1st October 2019. For the existing policyholders, the benefit shall be added after 1st October 2020. Most insurance policies do cover the surgery. You should contact your insurance provider to find out if your policy does provide coverage.
